Making Epidural Births Better
When preparing to birth your baby, one of the biggest questions on your mind is likely about pain management. The most common form of pain management in labor is epidural analgesia. You have probably heard from people around you that you should just get the epidural right away or “you don’t get a medal for going unmedicated,” or you might have heard that natural is best, an epidural will lead to a c-section, and you definitely shouldn’t get one. There is no one right answer to this question, and the answer for you might not be as black and white as you think. Before we talk about the evidence, risks, benefits, and alternatives to epidurals, let’s talk about what they actually are.
What is an epidural?
Epidural analgesia (the medical term for pain relief) is the name for the method used, not the medication itself.
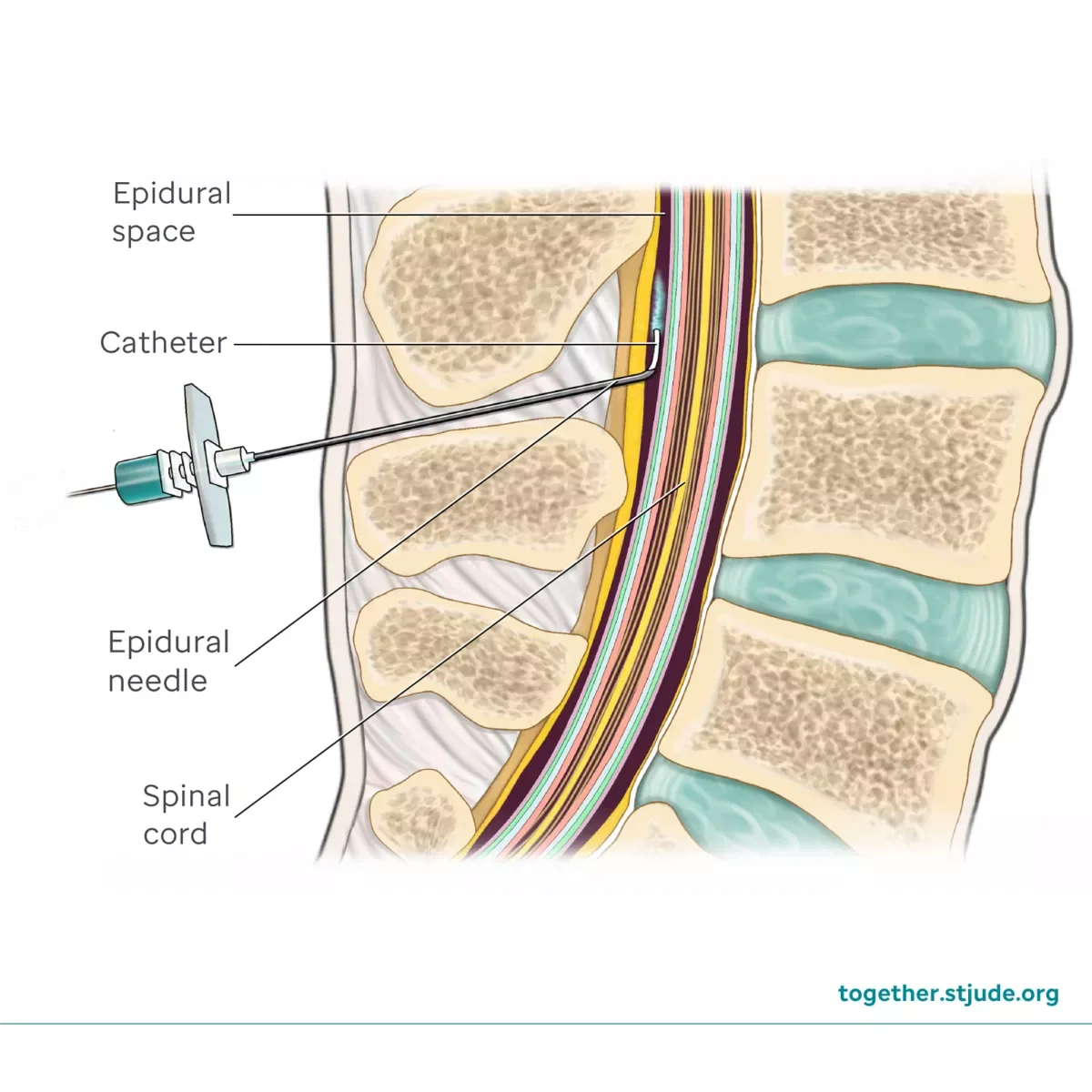
A small needle is used to find the space between the vertebrae of your spine in the lumbar region (lower back) and a small catheter (tube) is threaded through the needle into the space.
The epidural space, as pictured below, is composed of connective tissue, nerve roots, and blood vessels. When medications are administered here, they interact directly with the nerves. An almost undetectable amount enters the blood stream, making it a safe choice for labor pain management because not enough goes into the maternal bloodstream to have an effect on the baby directly.
An epidural usually uses two medications: one local anesthetic and one narcotic. I typically see bupivacaine and fentanyl.
Steps of an Epidural
When you request an epidural, the first thing your nurse will do is hook you up to a bag of IV fluids and bolus you with saline. This is to prevent you from having a dangerous blood pressure drop after receiving the epidural.
Once you have been bolused with fluids, the anesthesiologist or certified registered nurse anesthetist (CRNA) will enter your room and discuss risks and benefits of an epidural and have you sign consent forms.
To receive the epidural, the anesthesia provider will need access to your back, requiring you to hunch and bend over your belly. They may have you lean over a chair that is specially designed for this purpose, as pictured below.
The anesthesia provider will then clean and numb your back with a shot of lidocaine. Usually this is the most painful part, there is a pinch and then a burning sensation before the skin becomes numb.
Once the lidocaine has taken effect, they will use the needle to place the epidural catheter, then remove the needle and administer the first dose of medication. They will ask you to report any sensations of tingling or numbness in your legs, or a metallic taste in your mouth. Sometimes the catheter will be more to the left or right and they may have to remove it and try again. About 10-15% of people report ineffective epidurals, sometimes even with replacing the catheter they are still ineffective.
After the epidural has been placed, the anesthesia provider will tape it securely to your back. For the first 20-30 minutes, you will be instructed to lie on your back so that the medication doesn’t move more to one side or the other, since it flows with gravity. About 20 minutes after you receive an epidural, you should experience relief from your contractions.
After the epidural is placed, your blood pressure will be monitored frequently, because a common side effect of the medication is hypotension - or dangerously low blood pressure. Sometimes this can cause less blood flow to the placenta and baby, leading to fetal distress. Blood pressures are usually taken every 15 minutes from this point forward. You will also likely have a pulse oximeter on your finger, toe, or earlobe to monitor your pulse and oxygen saturation. You will also be on continuous IV fluids for the rest of your labor and immediate postpartum. Once you are numb, your nurse will place an indwelling Foley catheter in your bladder to drain urine, since you will no longer be able to walk to the bathroom or feel the urge to pee.
Once all of the boxes have been checked (your pain is managed, you’re stable, and all your tubes and wires are set up) you get the best part of an epidural: the nap!
Other Things to Know About Epidurals
You will not get complete relief from all labor sensations. You should not feel pain, but you will feel pressure. This becomes especially intense at the pushing stage.
You should still have some ability to move. You can move however you want, as long as you stay in bed. I have seen people be able to get into squats, lunges, all fours, and more with an epidural and some assistance.
If your epidural is too strong, you can ask to have it turned down.
The Foley catheter usually stays in until the baby’s head is visible. As an alternative, you can request the catheter to be removed before pushing and request intermittent catheterization if pushing is prolonged. Removing the indwelling catheter earlier may help to prevent mechanical damage to the bladder and urethra.
Pushing can take longer and be more difficult. It is common that when giving birth vaginally for the first time, it will take 1-3 hours, or longer with an epidural.
The medication should wear off by 2 hours after birth, when you will get up to use the bathroom for the first time.
Risks & Benefits
The following information is from Evidence Based Birth®
Benefits
The benefit of an epidural is usually relief from pain and the ability to rest.
For those exhausted from a long labor or induction, epidurals may help them rest, relax, and get some much-needed sleep
Effective pain management can reduce the maternal stress reaction and potentially improve blood supply and oxygen to the baby in some scenarios
In an emergency:
Having a functional epidural in place during labor can be beneficial if an urgent or emergency Cesarean is required.
• An existing epidural can be converted for surgery by adding a higher concentration of medication, which takes only about 10 minutes.
• This can be an advantage over needing a spinal block or general anesthesia if the epidural had not been placed prior to the emergency.
When compared to injectable opioids, epidural pain medications are considered safer for babies because there is a less direct route for the medication to enter the baby's body. An epidural did not impact the rate of Cesarean, the risk of severe perineal tears, backache, headache, itching, shivering, or drowsiness when compared to injectable opioids.
Risks
Low blood pressure (hypotension), 11 times the risk.
Fever, three times the risk.
Heavy motor block, causing extreme difficulty moving the lower parts of the body.
Itchy skin
Impact on Labor Progression and Delivery
Epidurals can increase the length of labor by about 32 minutes in the first stage and 15 minutes in the second stage.
Epidurals are linked to a longer second stage of labor (the pushing phase). One meta-analysis found participants with an epidural had five times the odds of experiencing a prolonged second stage. If the increased risk of needing forceps or vacuum was examined only using more recent studies (2005 onward), that increased risk disappeared, likely due to modern administration techniques like Patient-Controlled Analgesia (PCA) and lower doses.
A prolonged second stage led to five times the odds of having a vacuum or forceps-assisted birth in observational studies.
This lengthening of the second stage may be due to the epidural interrupting the utero-pituitary reflex, which normally strengthens contractions.
Rare Side Effects
Extremely rare complications include seizures, severe breathing difficulties, severe nerve damage, or death. Death from epidurals during labor is exceptionally rare, with one study over a 10-year period finding zero reported deaths.
Potential Effects on Breastfeeding
The research on epidurals and breastfeeding is conflicting. Researchers theorize negative effects can occur because:
The mother might develop a fever, potentially linked to lower Apgar scores and more difficulties for the newborn.
Excessive IV fluids used with epidurals can lead to painful breast swelling (engorgement), making breastfeeding more difficult.
Increased operative deliveries (vacuum/forceps) may delay skin-to-skin contact or cause neonatal bruising, hindering breastfeeding.
Specific evidence suggests that very high doses of epidural medications may negatively influence breastfeeding success. One trial found that babies whose mothers received a high dose of fentanyl had lower neurobehavior scores and those mothers were more likely to stop breastfeeding at six weeks postpartum compared to those who received low doses or no opioid.
(Note from Magdalena, not from EBB) Excessive IV fluids can also lead to increase in birth weight for baby, leading to a false high number. When baby quickly sheds this water weight, it can be calculated as a dangerous weight drop, potentially leading to formula being recommended when unnecessary.
Alternatives
The first alternative is seeing the amount of choices you have on this subject. This choice is not as black and white as you may imagine. At the extreme ends of the spectrum, some people feel that having an unmedicated birth is extremely important to them and would only consider it if it was life-saving. Others may feel so attached to having an epidural that a quick birth that did not allow for an epidural would leave them feeling very unsatisfied or traumatized by their birth experience, or their preference is to avoid all painful sensations in birth and to get an epidural as soon as possible. I see that people who are most satisfied with their birth experience are somewhere in the middle. Birth is wildly unpredictable and preparing and accepting the wide variety of ways your birth could go helps you remain informed and empowered no matter how it goes.
The range of feelings you may have about epidurals for pain management may be at the far ends of the spectrum, or they may be somewhere in the middle. You may:
Strongly prefer unmedicated labor and birth, but may consider epidural after long/exhausting labor.
Hope to birth unmedicated, but don’t feel like it’s that important to you.
Plan to labor without epidural at first, but eventually plan to get one unless birth progresses too fast.
Plan to get epidural on the sooner side after trying a few comfort measures.
If your beliefs fall towards the extreme ends of the spectrum, I encourage you to reflect and consider what your biases or fears are around this topic. Ultimately, epidurals are just another tool we have in our toolbox to get you to the end goal of a safe and satisfying birth experience and the choice whether or not to get one is deeply personal.
Alternative Methods of Pain Management
Injectable Opioids (read or watch Evidence Based Birth on IV opioids)
Nitrous Oxide (EBB handout)
Acupuncture or Acupressure (EBB on Acupuncture or Acupressure for Pain Relief)
Quiet Room
Soft Voices
Dim Lighting
Conscious or Guided Breathing
Hypnosis or Meditation
Massage, Counter Pressure, and Hip Squeezes
Music
Frequent Movement
Sterile Water Injections
TENS Unit
Shower or Tub
Words of Affirmation
The best approach to pain management involves using a variety of methods to manage the sensations of labor.
Sources and More Information
What is an epidural from Stony Brook Medicine University Associate in Obstetrics and Gynecology
From Evidence Based Birth®:
Epidural during Labor for Pain Management